Antibiotics were once the wonder drug. Now, however, an
increasing number of highly resistant -- and deadly -- bacteria are
spreading around the world. The killer bugs often originate in factory
farms, where animals are treated whether they are sick or not.
 |
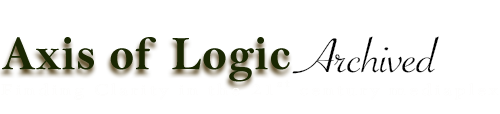
| An image of a strain of a Staphylococcus aureaus bacteria: Researchers around the world are growing increasingly worried about news strains of bacteria that are resistant to most common antibiotics. |
The pathogens thrive in warm, moist environments. They feel
comfortable in people's armpits, in the genital area and in the nasal
mucous membranes. Their hunting grounds are in the locker rooms of
schools and universities, as well as in the communal showers of prisons
and health clubs.
The bacteria are transmitted via the skin, through towels, clothing or
direct body contact. All it takes is a small abrasion to provide them
with access to a victim's bloodstream. Festering pustules develop at the
infection site, at which point the pathogens are also capable of
corroding the lungs. If doctors wait too long, patients can die very
quickly.
This is precisely what happened to Ashton Bonds, a 17-year-old
student at Staunton River High School in Bedford County, in the US state
of Virginia. Ashton spent a week fighting for his life -- and lost.
This is probably what also happened to Omar Rivera, a 12-year-old in New
York, who doctors sent home because they thought he was exhibiting
allergy symptoms. He died that same night.
The same thing almost happened at a high school in the town of Belen,
New Mexico. Less than two weeks ago, a cheerleader at the school was
hospitalized after complaining about an abscess. Twelve other female
students had been afflicted with suspicious rashes. All the students
tested positive for a bacterium that the US media has dubbed the
"superbug."
The school administration in Belen believes that the bacterium was
spread on mats in the school's fitness and wrestling rooms. The facility
was thoroughly disinfected 40 times, and yet the fear remains.
 |
| A MRSA (methicillin-resistant Staphylococcus aureus) bacteria strain is seen in a petri dish: Less than a century after the discovery of penicillin, one of the most powerful miracle weapons ever produced by modern medicine threatens to become ineffective.
|
Fears of a Pandemic
Microbiologists refer to this bacterium as community-acquired
methicillin-resistant Staphylococcus aureus, or ca-MRSA. The terrifying
thing about it is its resistance to almost all common antibiotics, which
complicates treatment. And, in contrast to the highly drug-resistant
hospital-acquired MRSA (ha-MRSA) strains, which primarily affect the
elderly and people in hospitals and nursing homes, ca-MRSA affects
healthy young people. The bacterium has become a serious health threat
in the United States. Doctors have already discovered it in Germany,
although no deaths have been attributed to it yet in the country.
The two bacteria, ha-MRSA and ca-MRSA, are only two strains from an
entire arsenal of pathogens that are now resistant to almost all
available antibiotics. Less than a century after the discovery of
penicillin, one of the most powerful miracle weapons ever produced by
modern medicine threatens to become ineffective.
The British medical journal The Lancet warns that the
drug-resistant bacteria could spark a "pandemic." And, in Germany, the
dangerous pathogens are no longer only feared "hospital bugs" found in
intensive care units (ICUs). Instead, they have become ubiquitous.
 |
| Some 900 metric tons of antibiotics are administered to livestock each year in Germany alone. Instead of treating only those animals that are truly sick, farmers routinely feed the medications to all of their animals. Likewise, some 300 metric tons of antibiotics are used to treat humans each year, far too often for those merely suffering from a common cold. This large-scale use inevitably leads to the spread of more resistant bacteria. |
About two weeks ago, consumers were alarmed by the results of an
analysis of chicken meat by the environmentalist group Friends of the
Earth Germany (BUND), which found multidrug-resistant bacteria on more
than half of the chicken parts purchased in supermarkets.
The dangerous bacteria have even been detected on one of Germany's
high-speed ICE trains. Likewise, more than 10 percent of the residents
of German retirement homes have been colonized by MRSA bacteria. In
their case, every open wound is potentially deadly. The pathogens have
also been found on beef, pork and vegetables.
Another alarming finding is that about 3 to 5 percent of the
population carries so-called ESBL-forming bacteria in the intestine
without knowing it. Even modern antibiotics are completely ineffective
against these highly resistant bacteria.
Diminishing Defenses
When the neonatal ICU at a hospital in the northern German city of
Bremen was infested with an ESBL-forming bacterium last fall, three
prematurely born babies died.
Infestation with multidrug-resistant bacteria is normally harmless to
healthy individuals because their immune systems can keep the pathogens
under control. Problems arise when an individual becomes seriously ill.
"Take, for example, a person who is having surgery and requires
artificial respiration and receives a venous or urinary catheter,"
explains Petra Gastmeier, director of the Institute of Hygiene and
Environmental Medicine at Berlin's Charité Hospital. "In such a case,
the resistant intestinal bacteria can enter the lungs, the bloodstream
and the bladder."
This results in urinary tract infections, pneumonia or sepsis, which
are increasingly only treatable with so-called reserve antibiotics, that
is, drugs for emergencies that should only be administered when common
antibiotics are no longer effective.
The Spread of Killer Bugs
Recently, an even greater threat has arisen. With the spread of
ESBL-forming bacteria, reserve antibiotics have to be used more and more
frequently, thereby allowing new resistances to develop. In fact, there
are already some pathogens that not even the drugs of last resort in
the medical arsenal can combat.
In India, where poor hygiene and the availability of over-the-counter
antibiotics encourage the development of resistance, an estimated 100 to
200 million people are reportedly already carriers of these virtually
unbeatable killer bacteria. There is only one antibiotic left -- a drug
that is normally not even used anymore owing to its potentially fatal
side effects -- that is still effective against these killer bacteria.
In serious cases, people who become infected with these types of
pathogens die of urinary tract infections, wound infections or
pneumonia.
The killer bugs have also reached England, presumably through medical
tourists who traveled to India for cosmetic surgery, and they have
reportedly already infected several hundred people. A few cases have
also turned up in Germany.
Israel even experienced a nationwide outbreak a few years ago. Within
a few months, about 1,300 people were afflicted by an extremely
dangerous bacterium that killed 40 percent of infected patients. Even
today, the same bacterium still sickens some 300 people a year.
Part 2: The Post Antibiotic Era
This rapid spread has caused many to wonder whether more and more
people in Germany will soon die of infectious diseases that were
supposedly treatable, as happened in centuries past. Unfortunately,
there are many indications that this might ultimately be the case.
"We are moving toward a post-antibiotic era," predicts Yehuda Carmeli
of the Tel Aviv Sourasky Medical Center. "But it won't happen on one
day or at the same time in every part of the world. And that's the
tragedy, because this means that it is not perceived as a serious
problem."
The World Health Organization (WHO) recently warned against an impending medical catastrophe. And, in The Lancet,
leading healthcare experts published an urgent appeal: "We have watched
too passively as the treasury of drugs that has served us well has been
stripped of its value. We urge our colleagues worldwide to take
responsibility for the protection of this precious resource. There is no
longer time for silence and complacency."
In fact, the carelessness with which doctors and farmers are
jeopardizing the effectiveness of one of the most important groups of
drugs borders on lunacy. Some 900 metric tons of antibiotics are
administered to livestock each year in Germany alone. Instead of
treating only those animals that are truly sick, farmers routinely feed
the medications to all of their animals. Likewise, some 300 metric tons
of antibiotics are used to treat humans each year, far too often for
those merely suffering from a common cold.
A Foe We Helped Become More Flexible
This large-scale use inevitably leads to the spread of resistant
bugs. Indeed, antibiotics offer ideal growth conditions to individual
bacteria that have naturally become resistant through a small change in
their genetic makeup. Simply put, they benefit from the fact that the
antibiotics still kill off their competitors, the non-resistant
bacteria.
In many cases, a genetic mutation isn't even necessary to allow a
resistant bacterium to develop. Bacteria can incorporate bits of genetic
material from other pathogens. For example, for millions of years, the
gene for ESBL resistance lay dormant in the ground, where it was part of
a complicated ecosystem of bacteria, penicillin-producing fungi and
plant roots. Again and again, the gene was incorporated by human
intestinal bacteria -- as useless ballast. It was only the large-scale
use of antibiotics that provided the ESBL-forming bacteria with the
opportunity to proliferate.
Recent studies show that quantities of antibiotics much smaller than
previously thought can lead to the development of resistance. In
retrospect, the uncontrolled dispensing of antibiotics has proven to be a
huge mistake. "In the last 30 years, we have contaminated our entire
environment with antibiotics and resistant bacteria," says Jan
Kluytmans, a microbiologist at Amphia Hospital, in the southern Dutch
city of Breda. "The question is whether this is even reversible anymore.
Perhaps we can prevent only the worst things from happening now."
Shocking Levels of Antibiotic Abuse on Farms
Since a large share of resistant bacteria come from barns, it will be
critical to drastically reduce the use of antibiotics in agriculture.
Remarkably often, farmers, feedlot operators and veterinarians are
themselves carriers of multidrug-resistant bacteria. Kluytmans has even
demonstrated that the pathogens found in humans are very often
genetically identical with the bacteria detected on meat.
It's virtually impossible to become infected by eating such meat, at
least as long as it's well-cooked. The risk arises when raw meat comes
into contact with small wounds. What's more, even vegetable crops can
become contaminated when liquid manure is spread onto fields.
The exhaust gases emitted by giant feedlots for pigs and chickens
could also pose a danger greater than previously thought. These meat
factories blow bacteria, viruses and fungi into the air. The government
of the western German state of North Rhine-Westphalia has commissioned a
study to determine whether feedlots are discharging multidrug-resistant
bacteria, thereby endangering people in the surrounding areas.
Last year, North Rhine-Westphalia was also the first German state to
systematically investigate the use of antibiotics in chicken farms. The
horrifying conclusion was that more than 96 percent of all animals had
received these drugs -- sometimes up to eight different agents -- in
their short lives of only a few weeks. "That was the proof that the
exception -- namely, treating disease -- had become the rule," says
Johannes Remmel, a Green Party member and the state's consumer
protection minister.
Abysmal Feedlot Conditions
As the results of the investigation suggest, factory farming is to
blame. The bigger an operation, the more antibiotics are administered to
individual animals. Investigators also noted that the duration of
antibiotic use was usually very short -- shorter than specified in the
licensing requirements. This saves money, but it also promotes the
formation of resistance.
The fact that livestock farmers mix antibiotics into feed has to do with production conditions in feedlots:
- To produce veal, animals from different sources that are too weak
for milk and beef production -- and likewise more susceptible to
infectious diseases -- are often jammed into enclosures.
- Pigs are usually kept in very small spaces, making them very
aggressive and causing them to fight. Their wounds have to be treated
with antibiotics.
- In the past, it took 80 days until a chicken was ready for
slaughter. Today it's only 37 days. Chicken farmers have a profit margin
of only a few cents per animal. To minimize losses through disease,
poultry producers and their veterinarian helpers use antibiotics as a
preventive tool.
However, factory farming is also possible without the uncontrolled
use of antibiotics. Dairy cows, for example, are usually not given these
drugs since antibiotics would interfere with the production of cheese
and yogurt. Nevertheless, there are still plenty of inexpensive milk
products on supermarket shelves.
"In the Netherlands," says Kluytmans, "the use of antibiotics in
feedlots was even reduced by about 30 percent within two years -- partly
as a result of stricter regulations for veterinarians. That's more than
we administer to humans." Unfortunately, he adds, the use of
antibiotics in feedlots is practically a matter of religious belief.
Efforts to Combat Antibiotics Abuse
In early January, Ilse Aigner, Germany's minister of food,
agriculture and consumer protection, unveiled a package of measures
aimed at curbing the use of antibiotics in farm animals. The measures
include stricter controls that would make it more difficult to add
antibiotics urgently needed in human medicine to animal feed. Germany's
federal government is also considering suspending veterinarians' right
to dispense medicine. In contrast to doctors practicing medicine on
humans, who prescribe drugs to be purchased at pharmacies, veterinarians
can even directly sell drugs to farmers and feedlot owners, which means
they stand to profit handsomely from the large-scale use of
antibiotics.
However, Remmel, the consumer protection minister of North
Rhine-Westphalia, believes that Aigner's proposals are "deceptively
packaged," and he is calling for exact specifications on the amounts of
antibiotics that can be used.
Similarly, there is also little control over the use of antibiotics
in human medicine. In Germany, in particular, doctors prescribe
antibiotics as they see fit, whereas in the Netherlands doctors must
first consult with a microbiologist.
"Just as in pain therapy, there really ought to be experts for
treatment with antibiotics," says Gastmeier, the director of the
Institute of Hygiene and Environmental Medicine at Berlin's Charité
Hospital "But young doctors, in particular, are often relatively
uninformed." Indeed, in medical school, they learn very little about the
proper use of antibiotics.
Little Research into New Antibiotics
Still, even more responsible prescribing practices will hardly be
able to stop the advance of resistant bacteria in the long term. What's
more, no new antibiotics can be seen on the horizon. Only four
pharmaceutical companies worldwide are still working on developing new
agents.
"Antibiotics have a serious problem," says Wolfgang Wohlleben of the
Institute of Microbiology at the University of Tübingen, in southwestern
Germany: "They actually work." Indeed, the drugs can get the better of
an infection within a few hours or days, and then they are no longer
needed. By contrast, patients taking drugs to fight high blood pressure
or diabetes often have to take them for the rest of their lives -- which
translates into steady, reliable profits for pharmaceutical companies.
Yet another factor making antibiotic-related R&D unattractive is
the fact that doctors can only prescribe a new antibiotic in the most
extreme of emergencies lest it lose its efficacy within a short amount
of time.
Given these circumstances, major pharmaceutical companies stopped
searching for new antibiotics years ago. Nowadays, only small start-ups
or university-based researchers are interested in the field.
Abandoned by Big Pharma
In reality, the search for new drugs should be getting easier rather
than more difficult. In the 1990s, the large pharmaceutical companies
spent several million euros searching for weaknesses in the genetic
makeup of bacteria. But although the researchers were actually
successful, the subsequently developed drugs never made the final leap
into clinical use.
"In the end, the risks of antibiotic research were simply too great
for companies," says pharmacist Julia Bandow, who went into academia to
continue studying antibiotics after working for the US-based
pharmaceutical giant Pfizer for six years.
But without the large pharmaceutical companies, there can be little
hope of progress. After all, testing a drug in human subjects takes
years and costs millions. And, as Bandow says of her fellow academics,
"We can't do it alone."
If pharmaceutical companies refuse to invest in the necessary
studies, it's critical for the government to step in. At the least,
politicians could make the development of antibiotics more attractive,
for example, by extending the time before patents expire so as to allow
companies to earn returns on their investments for longer. But, so far,
these are all nothing but ideas.
"At some point in the coming years," says microbiologist Kluytmans,
"there will be a disaster involving resistant pathogens with many
casualties. Only then will something change."
BY PHILIP BETHGE, VERONIKA HACKENBROCH, LAURA HÖFLINGER, MICHAEL LOECKX and UDO LUDWIG
Translated from the German by Christopher Sultan
Source: Der Spiegel